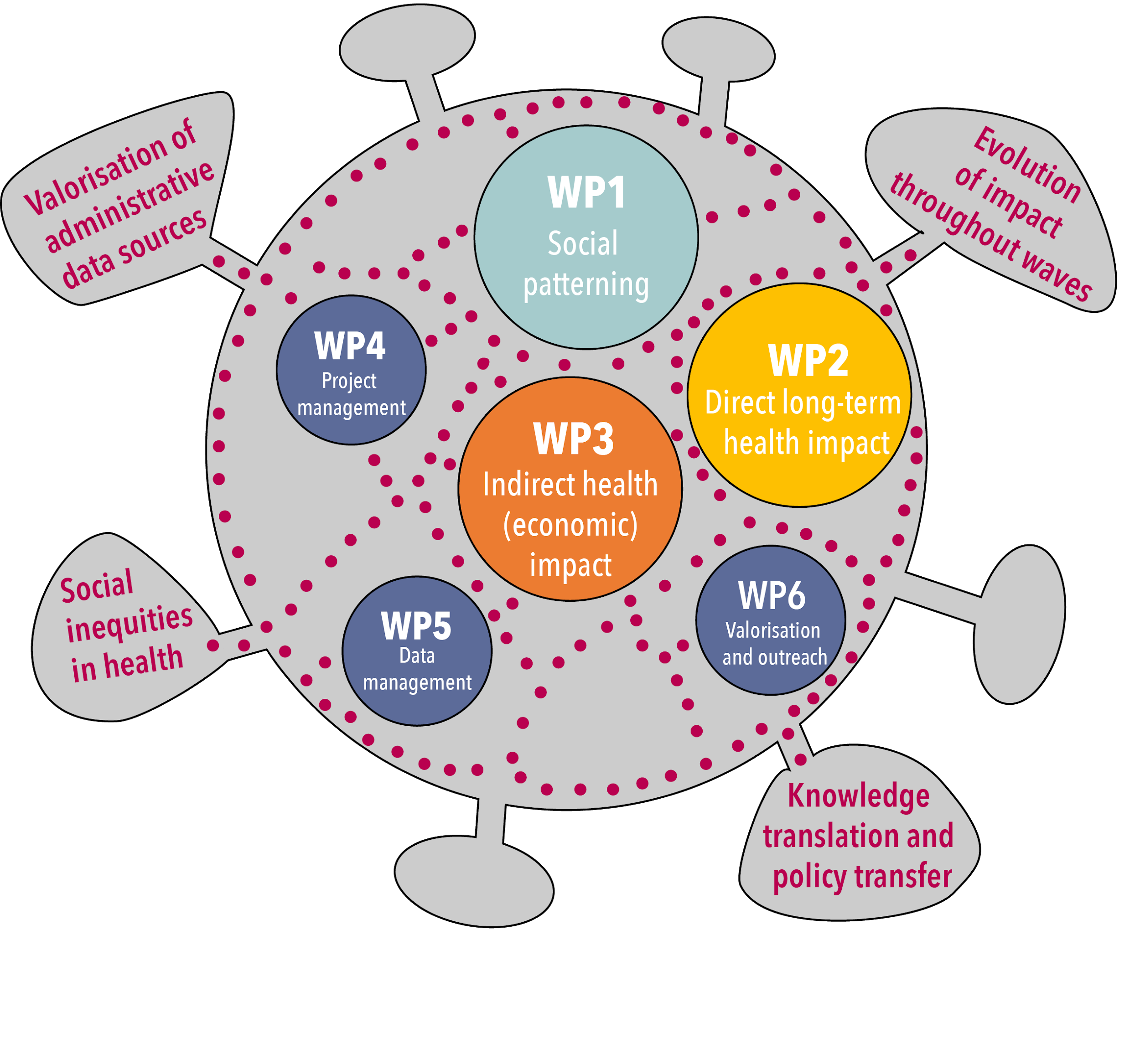
To accomplish its objectives, HELICON defines three scientific work packages. WP1 will focus on COVID-19 and the social patterning in various clinical stages of the disease so far. WP2 will investigate the direct long-term health impact of severe COVID-19 infections and develop methodological instruments for future investigations. WP3 will address the indirect health impact of the COVID-19 crisis on health care resource use and associated costs. Three support WPs are defined to facilitate the realisation of the three scientific WPs: WP4 will be dedicated to the project coordination, project management and reporting, WP5 will address the data management aspects of HELICON, and WP6 will ensure the valorisation, dissemination and exploitation of the results.
WP1: COVID-19 and social patterning
The social gradient in health and mortality has been well-established in international (e.g. Adler et al. 1994; Mackenbach et al. 2016) and Belgian research (e.g. Gadeyne & Deboosere 2002; Van den Borre & Deboosere 2018). Advantaged SE groups consistently have better health and live longer compared to disadvantaged groups. It is very likely that COVID-19 has exacerbated existing social health inequalities due the relationship between high SEPs and routes of exposure (e.g. ski-holidays, visiting family abroad). In addition, SEP is associated with key protective characteristics and infection preventative behaviour, e.g. higher levels of health literacy (Castro-Sánchez et al. 2016), reduced social networking time (Zhang and Xiang 2019) and smoking habits (Pampel et al. 2010). Furthermore, there may be social differences in how well the far-reaching corona containment measures have been abided. The aim of this WP is to investigate social inequalities with regard to COVID-19 testing, infection, hospitalization and mortality. The results will be used to develop an overview of vulnerable population groups helpful in targeted prevention and health care strategies. All subtasks will be achieved by analysing new linked data sourced in Stata MP 13.1 or higher with consideration of potential differences between waves of the epidemic.
WP1 addresses the following research questions:
- Is reimbursement of COVID-19 tests associated with SE/SD characteristics? If so, are there differences between waves? Compared to the general Belgian population, which SE/SD groups are not represented in the tested population?
- Is the spatio-temporal spread of COVID-19 infections related to SE/SD indicators?
- Is COVID-19 hospitalization associated with specific SE/SD characteristics? If so are there differences between waves? Compared to the general Belgian population, which SE/SD groups are not represented in the hospitalized population? Which SE/SD risk factors are related to intra-hospital outcomes (e.g., discharge, Intensive Care Unit (ICU) or death)?
- What are SE/SD risk factors to die due to COVID-19? Compared to the general Belgian population, which SE/SD protective factors are related to increased COVID-19 death risk? Are there differences in potential SE/SD mortality between waves of the COVID-19 epidemic?
WP2: Direct long-term health impact of COVID-19
To unravel the long-term health impacts of COVID-19 patients, HELICON will build on the results of the clinical survey of hospitalized COVID-19 patients conducted by Sciensano. As part of its federally established surveillance tasks in the context of public health, Sciensano has been tasked with establishing COVID-19 hospital surveys, covering both a monitoring of the hospital capacity and a clinical surveillance of hospitalized patients (Van Goethem et al. 2020). For the latter survey, Belgian hospitals were asked to provide coded individual data about their lab or CT-scan confirmed COVID-19 patients through an online survey on admission and discharge. These surveys gathered sociodemographic and medical information on patients, including comorbidities and other risk factors, their clinical course and their length of hospital stay. Ethical and legal (i.e. privacy protection) clearance for this surveillance was granted by the Commission for Medical Ethics of Ghent University Hospital (BC-07507) and by the Belgian Information Security Commission (CSI/CSSS/20/130), respectively.
Clinical follow-up of the patients after discharge is not currently foreseen, as it would be challenging both from a practical and financial point of view. As an alternative, we aim to make use of the rich health information landscape in Belgium to perform a follow-up based on administrative data sources. Specifically, we will link the hospital records to the health insurance data from IMA-AIM and the vital status data from Statbel.
WP2 addresses the following research questions:
- How did direct medical costs for hospitalized COVID-19 patients evolve during and after hospitalisation?
- What are long-term complications of COVID-19 patients after hospitalisation?
- What is the validity of the IMA-AIM “COVID-19 hospitalisation” code?
WP3: Indirect health economic impact of COVID-19 crisis
In addition to the direct health impact of COVID-19, the policy measures and behavioral changes in response the epidemic have had several indirect effects on population health. Planned non-urgent care was postponed, and patients restrained from medical care out of fear of becoming infected or hesitation because they assumed health care workers would be overwhelmed with COVID cases.
The aim of this WP is to investigate the potential indirect impact of the COVID-19 crisis in terms of Quality-Adjusted Life Year (QALY) losses, and changes in health care use and associated expenses, and productivity losses. These measures go beyond the simple descriptions of altered health care use, and are commonly used to assess the burden of disease, both nationally and internationally. They are of therefore of major value for adequate comparison across diseases and settings. By providing both the direct and indirect, medium- and long-term impact of COVID-19, policy makers will be able to weigh the risks, to make well-balanced and ethical decisions, considering the needs of all citizens. The applied methodology can also serve as guidance for future studies on the impact of conditions similar to the COVID-19 crisis on health-related quality of life, health care use and costs, and productivity losses. Finally, it provides a framework for future studies on the cost-effectiveness of measures taken during the COVID-19 crisis.
WP3 addresses the following research questions
- How did patterns of disease diagnosis change during the COVID-19 crisis?
- What are the changes in non-COVID-19 related causes of death during COVID-19 period compared with pre-COVID situation? Have mortality inequalities increased or reduced for other non-COVID causes of death?
- What is the health impact of delayed care due to the COVID-19 crisis in terms of Quality-Adjusted Life Years (QALYs)?
- What is the impact of delayed health care due to the COVID-19 crisis from a health-economic perspective?
WP4: Coordination, project management and reporting
HELICON will be coordinated by Sciensano (Prof Devleesschauwer), while the different partners will be responsible for the specific scientific work packages. To steer and monitor the progress of the different work packages, all partners will form a steering committee that will meet twice a year.
Reporting will be done as per Belspo requirements, including the elaboration of annual progress reports.
WP5: Data management
The HELICON project will establish linkages between a variety of data sources. Ethical and legal clearances will be submitted to the concerned parties.
WP6: Valorisation, dissemination and exploitation of the results
Valorisation will be at the heart of HELICON, with a major role set aside for the project website as central dissemination hub, and the follow-up committee as panel of key stakeholders. Issue and policy briefs will be written in preparation of the annual meetings with the committee. A dedicated technical report will be produced on methodology and use of administrative data (lessons learned and suggestions for improvement).

